In this article
2. Physical activity: Move intelligentlyFocus on:3. Stress and sleep management: Hormonal regulatorsManaging chronic stressOptimize sleepPCOS and severe premenstrual disordersBeware of sleep apnea4. Biomarkers to track: Measure to progressGlucose metabolism and insulin resistanceAndrogens and transportOvarian hormonesInflammationLiver functionLipid profileNutritional statusThyroidHow often?5. Supplementation: Targeted correctionThe essentialsWhat to remember about supplementationConclusion: Your roadmapIn this article
2. Physical activity: Move intelligentlyFocus on:3. Stress and sleep management: Hormonal regulatorsManaging chronic stressOptimize sleepPCOS and severe premenstrual disordersBeware of sleep apnea4. Biomarkers to track: Measure to progressGlucose metabolism and insulin resistanceAndrogens and transportOvarian hormonesInflammationLiver functionLipid profileNutritional statusThyroidHow often?5. Supplementation: Targeted correctionThe essentialsWhat to remember about supplementationConclusion: Your roadmap
PCOS Part 2: Concrete Solutions
Nutrition, activity, and sleep to better manage PCOS February 4, 2026In part one, we decoded PCOS mechanisms and why each woman has a unique profile. You now know that PCOS is a metabolic and hormonal syndrome that can be addressed by tackling underlying mechanisms.
Now, let's take action.
This second part presents concrete interventions to act on PCOS's main levers: insulin sensitivity, chronic inflammation, and hormonal balance.
Important: these recommendations don't replace medical follow-up. They constitute preventive and educational support to help you regain control of your metabolic and hormonal health.
Nutrition: The first lever (and the most powerful)
Diet directly affects insulin, inflammation, and androgen production. It's not about restriction, but construction: each meal is an opportunity to stabilize your metabolism.
1- Stabilize blood sugar
The goal is to reduce insulin spikes, even when blood sugar seems normal. At each meal, build your plate around four pillars:
Protein ~25-35g per meal: eggs, fish, poultry, tofu, tempeh, Greek yogurt or skyr if tolerated, legumes
Fiber: vegetables, whole fruits, legumes, seeds
Quality fats: olive oil, avocado, nuts, fatty fish
This combination slows carbohydrate absorption, stabilizes blood sugar, improves satiety, and reduces cravings.
Whole carbohydrates with low to moderate glycemic index: legumes, quinoa, buckwheat, sweet potato, basmati or brown rice if tolerated, whole fruits (particularly berries, kiwi, citrus).
2- Reduce inflammation through food
Increase whole foods
Favor gentle cooking methods
Integrate dietary omega-3s (sardines, mackerel, salmon)
Use anti-inflammatory spices (turmeric, ginger)
Consume polyphenols (berries, green tea)
Reduce alcohol consumption, added sugars, and processed foods
The real anti-inflammatory isn't an isolated superfood, it's daily repetition of coherent choices.
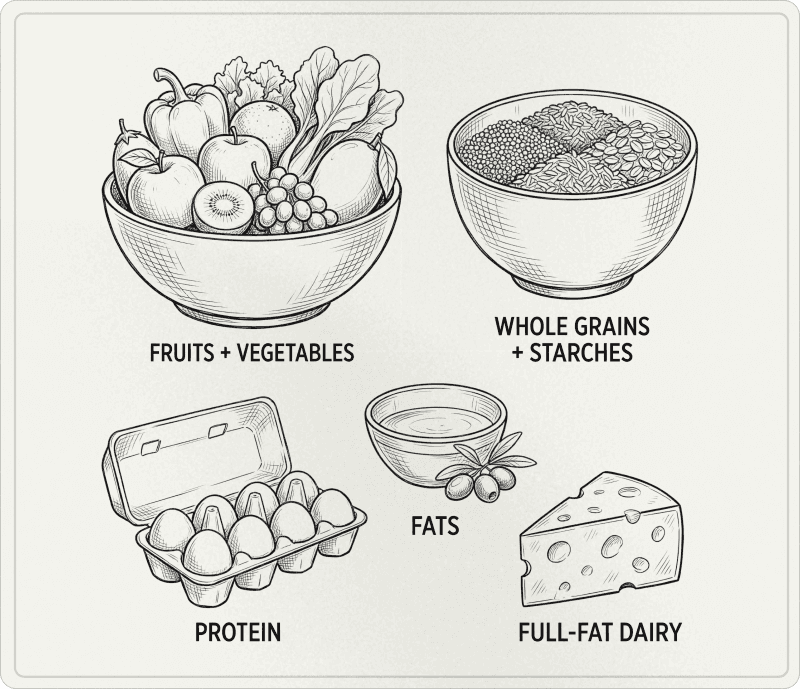
2. Physical activity: Move intelligently
Exercise improves insulin sensitivity and supports hormonal balance, independent of weight loss.
Focus on:
Strength training: 3-4 times per week
Strength training increases muscle mass, which directly improves glucose uptake and insulin sensitivity. Muscles are the main glucose reservoirs in the body.
Free weights, machines, bodyweight exercises (squats, lunges, push-ups, pull-ups). Aim for 30-45 minute sessions, with regular progression.
Daily walking: The underestimated weapon
Walking after meals (ideally 10-15 minutes) is simple, accessible, and very effective for regulating post-meal blood sugar without stressing the body. It's one of the most powerful and underused tools.
Some HIIT: Short and spaced
Sessions of 15-20 minutes maximum, 1-2 times per week. Short, intense intervals (20-30 seconds of intense effort, followed by 60-90 seconds of recovery) effectively improve insulin sensitivity without generating excessive stress.
If you have an adrenal profile or chronic stress, prioritize strength training and walking before adding HIIT.
What to avoid
Too many prolonged moderate-intensity cardio sessions that can worsen adrenal stress, particularly if you're already in a chronic stress situation. It seems counterintuitive, but more cardio of this type won't necessarily mean better results.
Overtraining. If your cycles lengthen, your sleep deteriorates, hunger explodes, and recovery is poor, it's not lack of willpower. It's often poorly calibrated training load. Balance is key: enough to stimulate, not too much to exhaust.
💡 Tracking tool: Heart Rate Variability (HRV)
HRV measures the interval between your heartbeats and reflects the state of your nervous system. It's an excellent indicator of recovery and stress tolerance:
High HRV = good recovery state, balanced nervous system, preserved stress tolerance
Low or declining HRV = signal of fatigue, chronic stress, insufficient recovery, potential overtraining
You can track your HRV with a watch or trackers like Whoop, Oura, connected devices. A progressive decline in your HRV over several days is a clear signal that you need to reduce training intensity or volume, prioritize rest, or improve your stress and sleep management.
3. Stress and sleep management: Hormonal regulators
Chronic stress and sleep deprivation directly disrupt your hormones, particularly cortisol, which worsens insulin resistance and stimulates DHEA-S production by the adrenals.
Managing chronic stress
International guidelines integrate mental health (anxiety, depression, body image, quality of life) as an evaluation and care axis for PCOS. It's not "in your head," it's biological reality.
Validated techniques:
Heart rate coherence: 5 minutes, 3 times daily (breathing: 5 seconds in, 5 seconds out). Reduces cortisol, improves heart rate variability.
Mindfulness meditation: 10-20 minutes daily. Reduces anxiety, improves emotional regulation, reduces inflammation.
Gentle or restorative yoga: activates parasympathetic nervous system (rest and repair), reduces cortisol.
Nature walks: 20-30 minutes daily. Reduces cortisol, improves mood.
Identify and reduce chronic stress sources
These techniques are important, but sometimes you need to identify and change the source: toxic relationship, work overload, perfectionism, social isolation. Identifying these factors is as important as any other nutritional or physical intervention.
Optimize sleep
Sleep deprivation (less than 7 hours per night) worsens insulin resistance, increases ghrelin (hunger hormone), reduces leptin (satiety), and disrupts hormonal production.
Sleep hygiene:
Regular schedule: go to bed and wake up at the same time, even on weekends
Reduce blue light: avoid screens 1-2h before bed, or use blue light blocking glasses
Cool temperature: 18-19°C in bedroom promotes sleep onset
Magnesium before bed: promotes relaxation and improves sleep quality
Calming routine: reading, herbal tea, gentle stretching, warm bath
PCOS and severe premenstrual disorders
Recent data suggest an association between PCOS and premenstrual dysphoric disorder (PMDD). If your premenstrual symptoms are very disabling, this deserves to be named, evaluated, and managed, not dismissed.
Beware of sleep apnea
The risk of obstructive sleep apnea is higher in women with PCOS. If you have snoring, daytime sleepiness, or restless sleep, talk to your doctor.
4. Biomarkers to track: Measure to progress
You can't improve what you don't measure. Identifying your hormonal and metabolic profile through precise biomarkers allows you to adjust interventions and track progress.
Glucose metabolism and insulin resistance
Fasting glucose, fasting insulin
HOMA-IR: calculated from fasting glucose and insulin
HbA1c: reflection of 3-month blood sugar
Androgens and transport
Total testosterone
Free testosterone
DHEA-S (adrenal origin)
SHBG
Ovarian hormones
LH and FSH: measured in early follicular phase (cycle day 2-5)
LH/FSH ratio: ratio >2 or 3 suggests PCOS, but not diagnostic alone
Inflammation
CRP (C-reactive protein): systemic inflammation marker
Liver function
ALT and AST
Lipid profile
Total cholesterol
LDL-C, HDL-C
Triglycerides
Nutritional status
Vitamin D (25-OH-vitamin D)
Magnesium
Ferritin
B12
Folate
Thyroid
TSH
Free T3
Free T4
PCOS often coexists with thyroid disorders (particularly Hashimoto's).
How often?
5. Supplementation: Targeted correction
Supplementation never replaces quality nutrition, but it can correct specific deficiencies and accelerate remission.
The essentials
Inositol (myo-inositol + D-chiro-inositol)
Myo-inositol ideally combined with D-chiro-inositol in a 40:1 ratio. Improves insulin sensitivity, reduces androgens, improves egg quality. Studies show benefits in some women, particularly on metabolic parameters and cycles.
Vitamin D3 (if deficient)
Deficiency is very common in women with PCOS (67-85%). The goal is to correct documented insufficiency. Improves insulin sensitivity, reduces inflammation, supports ovarian function.
Magnesium
Bioavailable forms: glycinate, bisglycinate, malate. Improves insulin sensitivity, reduces anxiety, improves sleep. In hyperinsulinemic profiles, urinary magnesium losses are greater.
Omega-3 (EPA + DHA)
Reduces inflammation, improves insulin sensitivity, improves lipid profile. Particularly relevant if triglycerides are elevated or fatty fish consumption is low.
What to remember about supplementation
Always test your biomarkers before and after to adjust
Favor quality: bioavailable forms, third-party tested brands
Don't take everything at once: start gradually and observe effects
Supplementation alone isn't enough, it accompanies adapted diet and lifestyle
Conclusion: Your roadmap
PCOS is a signal your body sends you, and you now have some keys to better understand it.
Your journey, step by step:
1. Consult a healthcare professional PCOS diagnosis and surveillance require medical support. Your doctor, gynecologist, endocrinologist, or midwife can:
Make the diagnosis
Exclude other causes (thyroid, hyperprolactinemia, etc.)
Prescribe appropriate biological tests
Ensure medical follow-up adapted to your situation
2. Get a complete panel of your biomarkers To identify your specific profile (glucose metabolism, androgen hormones, inflammation, liver, lipids, nutritional status, thyroid).
3. Implement preventive pillars
Nutrition: blood sugar stabilization and inflammation reduction
Physical activity: strength training + daily walking + activity adapted to your stress level
Sleep and stress: as important as nutrition
Targeted supplementation: based on your documented deficiencies and unique profile
4. Track your progress Reassess your biomarkers at 6 months to adjust your strategy.
PCOS symptom improvement is possible. It requires time, consistency, a comprehensive approach, and adapted medical support. But each adjustment you make is a step toward hormonal and metabolic balance.
You're taking back control.
This content is preventive and educational support that complements, and does not replace, medical follow-up.
Sources and Scientific References
Chen W, Pang Y. (2021). Metabolic Syndrome and PCOS: Pathogenesis and the Role of Metabolites. Metabolites, 11(12), 869.
Cooney LG, Dokras A. (2017). Psychological aspects of polycystic ovary syndrome. Seminars in Reproductive Medicine, 35(3), 238–248.
Dokras A, et al. (2011). Depression, anxiety and quality of life in women with polycystic ovary syndrome. Gynecological Endocrinology, 27(10), 787–793.
Dunaif A. (1997). Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Endocrine Reviews, 18(6), 774–800.
Escobar-Morreale HF, et al. (2005). The polycystic ovary syndrome associated with morbid obesity may resolve after weight loss induced by bariatric surgery. Journal of Clinical Endocrinology & Metabolism, 90(12), 6364–6369.
Greenwood EA, et al. (2018). Association of depression with the polycystic ovary syndrome symptom experience, quality of life, and body mass index. American Journal of Obstetrics and Gynecology, 219(4), 1–7.
Harrison CL, et al. (2011). Exercise therapy in polycystic ovary syndrome: a systematic review. Human Reproduction Update, 17(2), 171–183.
International PCOS Network. (2023). International evidence-based guideline for the assessment and management of polycystic ovary syndrome 2023. Monash University (MCHRI).
Joham AE, et al. (2022). Polycystic ovary syndrome. The Lancet Diabetes & Endocrinology, 10(9), 668–680.
Legro RS, et al. (2013). Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. Journal of Clinical Endocrinology & Metabolism, 98(12), 4565–4592.
March WA, et al. (2010). The prevalence and features of the polycystic ovary syndrome in an unselected population. Journal of Clinical Endocrinology & Metabolism, 95(5), 2038–2049.
Moran LJ, et al. (2010). Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Human Reproduction Update, 16(4), 347–363.
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. (2004). Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertility and Sterility, 81(1), 19–25.
Soffer D, et al. (2024). Role of apoB in clinical management of cardiovascular risk in adults: an expert clinical consensus from the National Lipid Association. Journal of Clinical Lipidology.
