In this article
Low libido: causes, tests, solutionsTHE MOST COMMON CAUSES1) Medications (very common cause, often overlooked)2) Hormonal imbalancesTestosteroneEstrogensThyroid3) Metabolism, blood sugar, vascular health4) Chronic stress, cortisol, and nervous system: libido requires safety5) Sleep debt (often a determining factor)6) Chronic inflammation (the body prioritizes urgency)7) Micronutrient deficiencies (energy, neurotransmitters, steroidogenesis)8) Life phases where libido frequently dropsPostpartum and breastfeedingPerimenopause and menopauseAge-related testosterone declineSOLUTIONS: RESTORING THE FOUNDATIONSSOLUTIONS: START BY RESTORING THE FOUNDATIONSStep 1: Reinstall physiological safety (sleep + stress)Sleep: the foundationStress: reduce the "background noise"Step 2: Restore available energy (nutrition + intake)Blood sugar stabilityAdequate intake (avoid under-eating)Correct identified deficienciesStep 3: Circulation and movementStrength trainingDaily movement: 20 to 30 minutesAvoid overtrainingStep 4: Eliminate physical barriers and consult if neededPhysical comfort (eliminate pain)When to consult a mental health professional?When to see a doctor?In this article
Low libido: causes, tests, solutionsTHE MOST COMMON CAUSES1) Medications (very common cause, often overlooked)2) Hormonal imbalancesTestosteroneEstrogensThyroid3) Metabolism, blood sugar, vascular health4) Chronic stress, cortisol, and nervous system: libido requires safety5) Sleep debt (often a determining factor)6) Chronic inflammation (the body prioritizes urgency)7) Micronutrient deficiencies (energy, neurotransmitters, steroidogenesis)8) Life phases where libido frequently dropsPostpartum and breastfeedingPerimenopause and menopauseAge-related testosterone declineSOLUTIONS: RESTORING THE FOUNDATIONSSOLUTIONS: START BY RESTORING THE FOUNDATIONSStep 1: Reinstall physiological safety (sleep + stress)Sleep: the foundationStress: reduce the "background noise"Step 2: Restore available energy (nutrition + intake)Blood sugar stabilityAdequate intake (avoid under-eating)Correct identified deficienciesStep 3: Circulation and movementStrength trainingDaily movement: 20 to 30 minutesAvoid overtrainingStep 4: Eliminate physical barriers and consult if neededPhysical comfort (eliminate pain)When to consult a mental health professional?When to see a doctor?
Your libido is a health biomarker (part 2)
Low libido: causes, tests, solutionsFebruary 20, 2026Low libido: causes, tests, solutions
Understanding the signal. Testing what matters. Restoring the foundations.
In part 1, we established a key point: libido is a biological function that depends on multiple systems (brain, nervous system, circulation, hormones, metabolism).
In this blogpost, we're going further, with three simple objectives:
Understanding the most common causes of low libido (women and men)
Identifying the truly useful biomarkers to objectify the signal
Prioritizing concrete actions to rebuild the foundations
Because a sustained drop in libido can reflect a hormonal, metabolic, vascular, inflammatory, or nervous imbalance — and it deserves to be taken seriously.
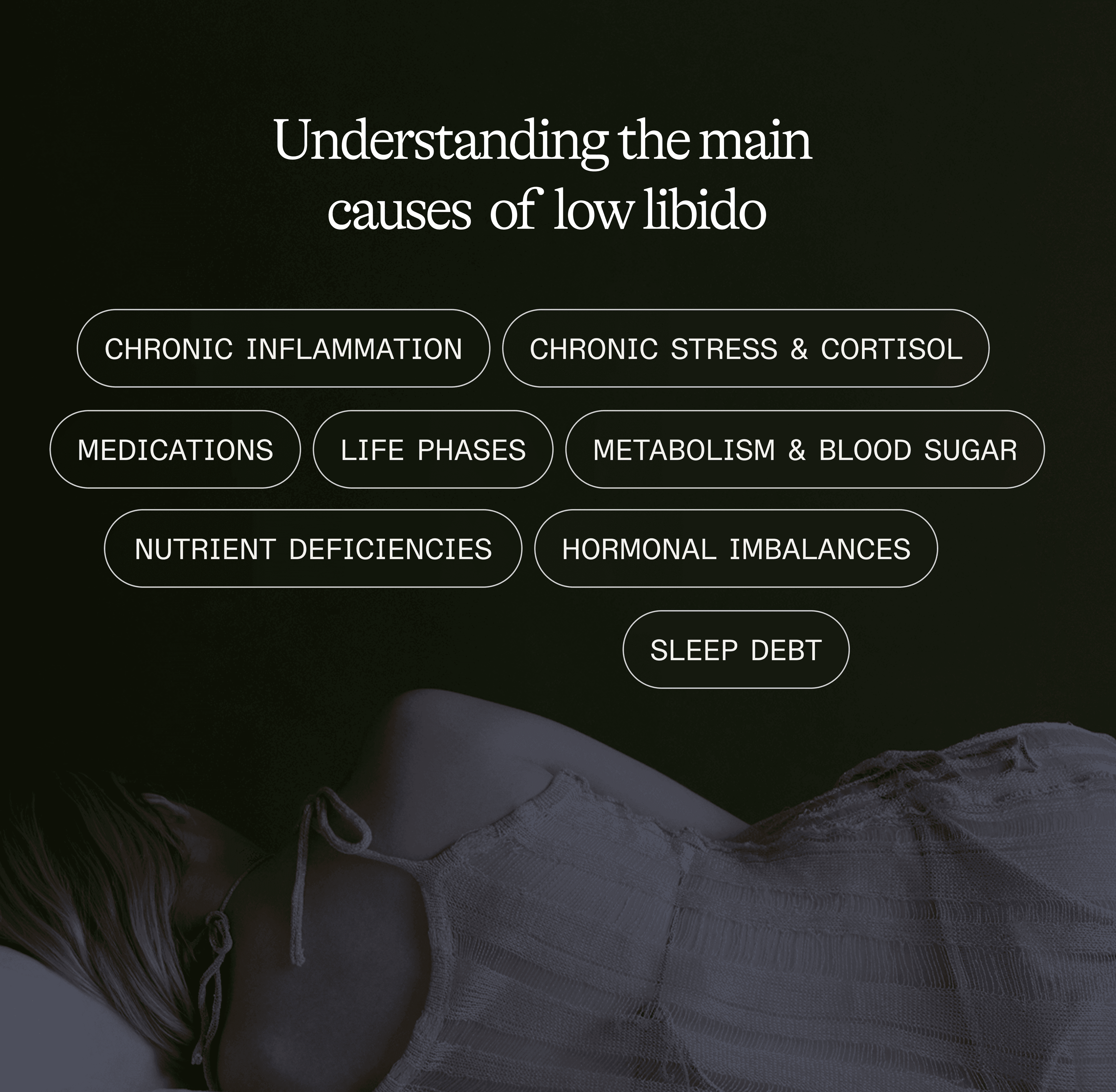
THE MOST COMMON CAUSES
1) Medications (very common cause, often overlooked)
SSRIs / antidepressants
SSRIs increase serotonin availability. From a sexual standpoint, this can:
reduce dopaminergic activity involved in motivation and "drive"
decrease arousal (physical and mental)
make orgasm more difficult or less intense
Classic result: decreased desire, slower arousal, less accessible orgasms.
Hormonal contraception (pill and similar)
Two physiological mechanisms explain a sometimes "flatter" libido:
Suppression of ovulation: disappearance of the physiological estradiol peak mid-cycle, often associated with increased desire in some women
Increase in SHBG: SHBG binds testosterone and reduces the free (bioavailable) fraction
Possible consequence: less spontaneous drive, less reactivity, less "instinctive" desire.
2) Hormonal imbalances
Testosterone
The drive hormone: initiative, spontaneous desire, reactivity to pleasure.
In men: it decreases by 1-2%/year after age 30 and depends heavily on sleep, with a morning peak produced during deep sleep.
In women: levels are lower than in men, but its role is crucial for desire, arousal, sensitivity, and satisfaction. The pill, stress, and lack of sleep reduce bioavailability by increasing SHBG or stopping ovarian production.
When it drops: less spontaneous desire, need for more stimulation to "trigger" interest.
Biomarkers to monitor:
Total testosterone
Free testosterone
SHBG
Estrogens
In women: they ensure genital vascularization, lubrication, and sensitivity. The estradiol peak before ovulation coincides with a desire peak in about 60% of women. In menopause, the sudden drop in estrogens leads to dryness, pain, and less tissue comfort, which mechanically reduces desire.
In men: estrogens are necessary but an excess (produced by aromatase from abdominal adipose tissue) creates an imbalance.
More abdominal fat = more aromatase = more conversion of testosterone to estradiol. Excess estradiol then reduces testosterone production.
It's a vicious circle: abdominal overweight → more aromatase → less testosterone → harder to maintain muscle mass → easier to store fat → even less testosterone.
Thyroid
Your thyroid is your metabolic thermostat: energy, mood, circulation, follicular development. When it slows down, everything slows down.
50% of hypothyroid women report low libido.
The most common symptoms: fatigue, feeling cold, brain fog, weight gain, irregular cycles.
A test limited to TSH can miss a free T3 deficit. A complete panel is necessary:
TSH
Free T3
Free T4
3) Metabolism, blood sugar, vascular health
Libido is also a matter of circulation.
Sexual arousal depends on a vascular mechanism: genital tissues need sufficient blood flow to ensure engorgement, sensitivity, and lubrication (women) or erection (men). This vasodilation relies on nitric oxide (NO) production, a molecule released by the endothelium (inner wall of blood vessels).
An unfavorable cardiometabolic terrain (unstable blood sugar, insulin resistance, chronic inflammation, abdominal overweight) can damage the endothelium and reduce nitric oxide production. Less NO = less vasodilation = less blood flow = less reliable and less intense physiological response.
In men, erectile dysfunction can be an early cardiovascular signal — a warning sign to take seriously.
Metabolic signs to watch: high waist circumference, post-meal fatigue, frequent sugar cravings.
Biomarkers to monitor:
Fasting blood glucose
HbA1c
Fasting insulin
HOMA-IR index
4) Chronic stress, cortisol, and nervous system: libido requires safety
Sexuality requires the ability to shift to the parasympathetic nervous system (relaxation, safety).
Under chronic stress:
the nervous system stays in alert mode
sleep becomes fragmented
recovery decreases
mental and physical availability drops
In a body in survival mode, desire becomes secondary.
Common signals: nighttime awakenings, rumination, irritability, morning fatigue, difficult recovery, abdominal storage, irregular cycles in women.
Biomarkers to monitor: CAR (Cortisol Awakening Response): Cortisol profile at 0-30-60 min after waking. Assesses stress axis reactivity and recovery capacity.
5) Sleep debt (often a determining factor)
Sleep is the active restoration phase for multiple interconnected systems:
the hormonal system (including testosterone production in men),
the nervous system (stress, anxiety, and irritability regulation),
metabolism (appetite and blood sugar management),
and emotional balance (motivation, ability to feel pleasure).
Without quality sleep, all these systems gradually dysregulate, and libido becomes one of the first victims.
6) Chronic inflammation (the body prioritizes urgency)
Low-grade inflammation consumes resources: it mobilizes immunity, disrupts recovery, and can influence hormonal balance and perceived energy.
When the body is "managing a fire," it invests less in non-vital functions, including sexuality.
Common causes: ultra-processed foods, alcohol, lack of sleep, stress, dysbiosis, persistent infections, overtraining without recovery.
Biomarkers to monitor:
High-sensitivity CRP (hs-CRP)
Oxidized LDL
7) Micronutrient deficiencies (energy, neurotransmitters, steroidogenesis)
Libido depends on cellular energy, neurotransmission (especially dopamine), and the body's ability to produce/balance hormones. Certain deficiencies can...
Common deficiencies to screen via blood test:
Iron / ferritin: Oxygen transport, energy production. Deficit = fatigue, shortness of breath, anxiety, low libido.
Vitamin D: Steroid hormone with receptors in hypothalamus, ovaries, testicles. Deficit = depression, fatigue, sexual dysfunction.
Magnesium: Cofactor for 300+ enzymatic reactions. Stress management, relaxation, sleep. Very common deficit.
Zinc: Testosterone → DHT conversion (active form). Hormonal production, immunity.
8) Life phases where libido frequently drops
Postpartum and breastfeeding
After childbirth, hormones drop abruptly. This hormonal drop often creates vaginal dryness and reduced tissue sensitivity.
If the woman is breastfeeding, prolactin remains elevated, which inhibits the reproductive hormonal axis. Add to this massive sleep debt, significant mental load, and sometimes pain related to physical recovery.
Result: a frequent and biologically coherent drop in libido, which can last 6 to 18 months. It's a normal physiological response.
Perimenopause and menopause
In perimenopause, cycles become irregular and hormones fluctuate erratically. In menopause, estrogens drop definitively, leading to vaginal dryness, tissue atrophy, and possible pain during intercourse.
Sleep is often disrupted, which worsens fatigue and further reduces desire. Less comfort = less pleasure = less desire. It's a vicious circle that many menopausal women experience.
Age-related testosterone decline
In men, testosterone gradually decreases by 1 to 2% per year after age 30. This decline leads to less spontaneous desire, more fatigue, muscle mass loss, increased abdominal fat, and sometimes erectile difficulties.
Sleep apnea often worsens the picture: sleep fragmentation prevents nighttime testosterone production. Abdominal overweight also creates a vicious circle.
Finally, chronic stress and lack of sleep slow down the hormonal axis. Low libido in men is therefore not just a matter of age: it's often a cumulation of hormonal, vascular, metabolic, and nervous factors (stress, sleep).
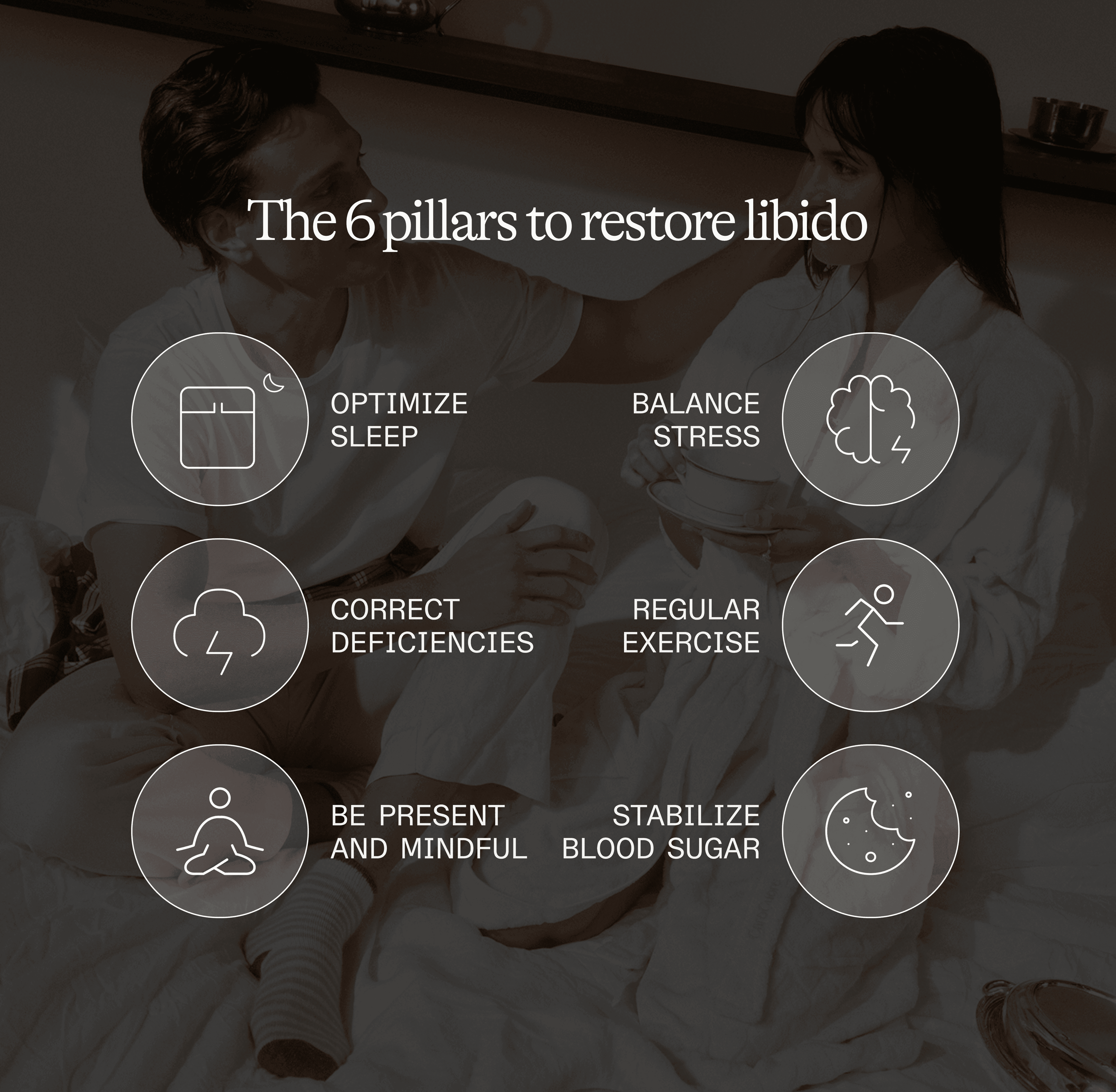
SOLUTIONS: RESTORING THE FOUNDATIONS
The goal is to put the body back into a state where desire becomes possible again.
SOLUTIONS: START BY RESTORING THE FOUNDATIONS
Step 1: Reinstall physiological safety (sleep + stress)
Libido needs a body that can shift to parasympathetic (relaxation, recovery).
Sleep: the foundation
→ Aim for 7 to 9h per night when possible. Keeping regular bedtime and wake time, even on weekends, stabilizes circadian rhythm.
→ Go to bed before 11pm: the melatonin peak occurs between 10pm and 2am. Going to bed after midnight means missing part of this window.
→ Cool room (18-19°C/64-66°F), dark (blackout curtains or mask), and no screens 1h before bed. Blue light suppresses melatonin.
→ If sleep remains fragmented: first treat the causes (stress, alcohol, late dinner, sleep apnea, overtraining, chronic pain).
Stress: reduce the "background noise"
→ Micro breathing pauses: 2 to 3 minutes, several times a day, with exhalation longer than inhalation. This activates the vagus nerve and reduces cortisol.
→ Daily walk: 20 to 30 minutes, ideally in nature or outdoors. It's a natural anti-inflammatory and helps metabolize cortisol.
→ Morning daylight exposure: within 30 minutes after waking. This stabilizes circadian rhythm and improves evening sleep.
→ Time for yourself: protect "demand-free" time. The nervous system needs real recovery phases, not just sleep.
Goal: Regain a less reactive nervous system, deeper recovery, and physical availability for arousal.
Step 2: Restore available energy (nutrition + intake)
Blood sugar stability
→ Protein at each meal: 25-30 g (meat, fish, eggs, legumes). Starting the meal with protein stabilizes blood sugar.
→ Fiber and good fats: vegetables, seeds, nuts, olive oil, avocado. They slow carbohydrate absorption and nourish the microbiome.
→ Limit added sugars: less than 25 g per day. Avoid ultra-processed foods that create blood sugar spikes followed by sharp drops.
→ Short post-meal walk: 10 to 15 minutes within 30 minutes after a meal can reduce blood sugar by 20 to 30%.
Adequate intake (avoid under-eating)
A collapsing libido can be a signal of insufficient energy availability. This occurs when caloric intake is too low relative to total expenditure (basal metabolism + daily activity + training).
The body then perceives an energy threat and puts non-vital functions on standby, including reproduction. Result: decreased or stopped libido, irregular or absent cycles in women (amenorrhea), decreased testosterone in men.
Signs of chronic under-eating:
→ Persistent fatigue despite rest
→ Difficult recovery after exercise
→ Constant coldness (hands, feet)
→ Disrupted sleep
→ Irritability, anxiety
→ Muscle mass loss despite training
→ Drop in libido, disrupted cycles (women), erectile difficulty (men)
Common in: female athletes, people in prolonged caloric restriction.
Correct identified deficiencies
If your blood test reveals deficiencies (iron, vitamin D, magnesium, zinc), correcting them in a targeted way can restore energy, mood, and hormonal function.
Principle: Supplement according to test results, not "randomly." Excess can create other imbalances (e.g., too much zinc inhibits copper absorption).
Smart approach:
Test first: complete blood panel
Correct what's missing according to recommendations
Retest after 3 months: verify levels normalize, adjust or stop according to results
Don't over-supplement: vitamins and minerals work in synergy and balance
A body with enough energy and resources can invest in sexual function, biologically considered non-vital if the foundations aren't solid.
Step 3: Circulation and movement
Exercise improves vascular function (nitric oxide production), insulin sensitivity, testosterone production, and body composition.
Strength training
→ ≥ 3 times per week: squats, deadlifts, push-ups, pull-ups — large muscle groups stimulate testosterone the most.
→ Benefits: improves insulin sensitivity, temporarily boosts testosterone, maintains muscle mass, optimizes circulation.
Daily movement: 20 to 30 minutes
→ Types: walking, cycling, swimming, gentle yoga.
→ Benefits: improves endothelial function (vessel capacity to produce nitric oxide), reduces chronic inflammation, helps metabolize cortisol.
Avoid overtraining
→ The risk: too much intensity without recovery produces the opposite effect: nervous fatigue, chronically elevated cortisol, dropping testosterone, collapsing libido.
→ Warning signs: persistent fatigue despite rest, irritability, disrupted sleep, performance decline, frequent infections, low libido.
Step 4: Eliminate physical barriers and consult if needed
Physical comfort (eliminate pain)
If intercourse is associated with pain, dryness, or discomfort, the body anticipates pain and cuts off desire to protect itself. It's a biological defense mechanism, not a "lack of willpower."
Treat the cause with a professional:
→ Vaginal dryness/atrophy (common in menopause): local estrogens (cream, suppositories), lubricants during intercourse, regular vaginal moisturizers (2-3x/week).
→ Pain during intercourse: gynecological consultation to rule out or treat endometriosis, vaginismus, infections, or postpartum scars.
Comfort is non-negotiable. No pleasure without comfort. No desire without pleasure.
When to consult a mental health professional?
→ Emotional distress (persistent anxiety, depression)
→ History of trauma impacting sexuality
→ Significant relationship difficulties
→ Deep guilt or shame around sexuality
When to see a doctor?
→ Sudden and unexplained drop in libido that persists
→ Pain during intercourse
→ Symptoms of hormonal dysfunction
→ Suspicion of medication impact
A drop in libido is never "just in your head."
It's a physiological signal as legitimate as fatigue, deteriorating sleep, or changing cycles.
With Lucis, you can get out of the fog:
measure the biomarkers that influence desire (hormones, thyroid, inflammation, energy, metabolism)
receive a clear, contextualized reading
identify the priority lever (instead of randomly piling up solutions)
The information in this blog is provided for educational purposes only and does not replace medical advice. For any health questions, persistent symptoms, or pain, consult a qualified healthcare professional.
References
Argiolas, A., & Melis, M. R. (1995). Neuromodulation of penile erection: An overview of the role of neurotransmitters and neuropeptides. Progress in Neurobiology, 47(4–5), 235–255.
Dominguez, J. M., & Hull, E. M. (2005). Dopamine, the medial preoptic area, and male sexual behavior. Physiology & Behavior, 86(3), 356–368.
Georgiadis, J. R., & Kringelbach, M. L. (2012). The human sexual response cycle: Brain imaging evidence linking sex to other pleasures. Progress in Neurobiology, 98(1), 49–81.
Hull, E. M., Muschamp, J. W., & Sato, S. (2004). Dopamine and serotonin: Influences on male sexual behavior. Physiology & Behavior, 83(2), 291–307.
Levin, R. J. (2003). The ins and outs of vaginal lubrication. Sexual and Relationship Therapy, 18(4), 509–513.
McKenna, K. (1999). The brain is the master organ in sexual function: Central nervous system control of male and female sexual function. International Journal of Impotence Research, 11(Suppl 1), S48–S55.
Meston, C. M., & Frohlich, P. F. (2000). The neurobiology of sexual function. Archives of General Psychiatry, 57(11), 1012–1030.
Pfaus, J. G. (2009). Pathways of sexual desire. The Journal of Sexual Medicine, 6(6), 1506–1533.
Stoléru, S., Fonteille, V., Cornélis, C., Joyal, C., & Moulier, V. (2012). Functional neuroimaging studies of sexual arousal and orgasm in healthy men and women: A review and meta-analysis. Neuroscience & Biobehavioral Reviews, 36(6), 1481–1509.
